Testicular cancer
A rare tumor
Testicle cancer is a rare tumor affecting 2 320 new cases each year. Medical progress have made it possible to decrease its death rate by 40% since 1990’s and reach an almost 90% recovery rate.
Thus it is a cancer with a favorable prognosis, even in its metastatic form.
This cancer is the most common among young men with an incidence peak between 15 and 34 years old. Nevertheless it can be detected at any age.
It mainly has to do with patients with medical history such as :
- cryptorchidism : it corresponds to the absence of one or both testes from the scrotum
- testicular atrophy
- hypospadias: it is a condition present from birth in which the opening of a boy's urethra isn't located at the tip of the penis.
- fertility disorders
The medical examination performed by the doctor is based upon a palpation of the testes in order to identify a nodule and the search for lymph nodes by a palpation of ganglionic areas. Doppler ultrasound of the testis is a simple and painless imaging system that enables to déterminer the size, the number and the exact location of lesions. The final diagnosis on the testicle analysis can only be made after the operation.
A chest and abdomen scanner with injection of a contrast agent must be performed before or just after the operation to check for the presence of lymph nodes or metastases. Testicular cancer cells mainly spread to the lymph glands that run alongside the aorta and to the lungs or the brain. In case of scanner contraindication (iodine allergy, renal failure) it is possible to perform an MRI.
Other tests such as a bone or brain scanner can be performed on a case-by-case basis depending on the context and the results of the ultrasound and scanner.
A blood test must be performed before and after the operation, it consists of a dosage of 3 markers : total hCG, alpha-fetoprotein (AFP), LDH. These markers are used to to determine the stage and prognosis (chance of recovery). In case there is no normalization of these markers, the disease is considered as a metastatic disease and a chemotherapy treatment is given right after the operation.
Patient care and treatment process
The Colmar Hospital Centre is able to greet patients suspected of having testicular cancer in its polyclinic during the whole week and on Saturday mornings in order to ensure a fast and efficient patient care process.
The doctor updates the medical examinations and the biology tests and schedules a surgery date in semi-emergency (1 to 2 weeks delay). An information sheet containing all the data related to sperm storage at the CECOS (centre for the study and storage of oocytes and sperm) is given to him.
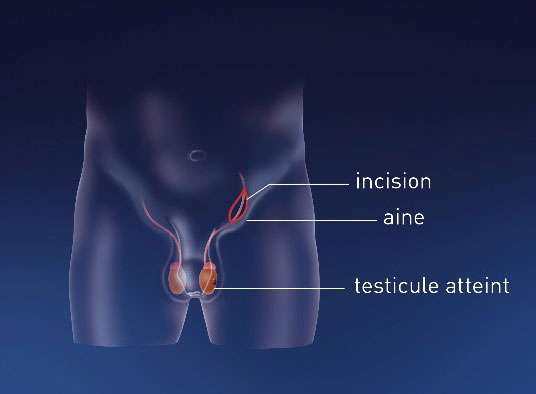
The removal of the affected testicle (also called orchiectomy) is the first step of the treatment.
An inguinal incision is performed and the spermatic cord is clamped off in order to avoid tumor invasion.
The excised tissues will then be analyzed in order to assess the exact type of tumor.
Depending on the choice of the patient, a testicular prosthesis made of silicone can be implanted during the same surgery time. The size of this prosthesis will be adapted to the remaining testicle’s one. This operation can also be performed afterwards.

Potential adverse effects and surgical follow-up
The main potential adverse effects related to this intervention are :
– Hematoma
– Infection
– Inguinal hernia
– Trauma of the ilioinguinal nerve which can result in pains or anaesthesia at the top of the thigh and scrotum. These symptoms are usually regressive.
These effects are rather rare but they may require a specific patient care.
In case the patient needs to urgently start a chemotherapy, surgery can be deffered and performed later on.
Depending on the tumor type and the stage of the disease, a radiotherapy or a chemotherapy may be carried out. These therapies options are discussed on a case-by-case basis during multidisciplinary meetings in order to ensure a specific and well-adapted patient care process.
A close surveillance of the patient is vital during the first two years and later on during the rest of his life. It consists in the completion of Thoracic-Abdominal-Pelvic scanner and blood marker tests. Their frequency depends on the tumor type and stage of the disease.